Cancer Treatment

Interventional Oncology
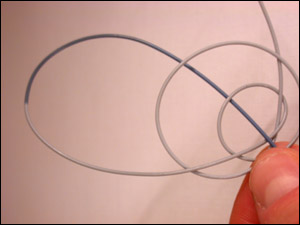
Interventional radiology techniques are quickly becoming standard therapies for cancer treatment. Interventional oncology is the name for this new, high tech and evolving field of non-sugical cancer therapy. An arsenal of tools has become integral to tumor diagnosis, treatment, pain control and palliation for our interventional oncology team in Illinois. Our team of highly skilled image-guided doctors can deliver cutting edge treatment deep inside the body to kill cancer without open surgery. For example we can use Microcatheters (see photo below for scale) to travel through arteries or veins to the site of cancer, and release treatment agents locally at the cancer site.

Liver directed therapies
For patients with primary liver cancers or cancers that involve the liver (such as those from the colon, stomach, pancreas, and breast), there are many treatment options that we offer in addition to chemotherapy, radiation, and surgery. These can be broken down into: radioembolization (Y-90), Chemoembolization, and Thermal Ablation.
Radioembolization (Y-90)
An exciting new liver cancer treatment offered by our group is Yttrium-90 microsphere therapy for liver tumors. A tiny catheter is threaded into the liver artery, then microscopic glass beads impregnated with a highly radioactive element are injected into the liver tumors, giving them a higher dose of radiation than can be safely delivered by external beam radiation treatment. There are only about 40 centers performing this treatment in the USA at this time, including our clinic in Illinois. This liver cancer treatment is effective against primary cancer of the liver, but new research is showing that it can be effective in treating metastatic cancer in the liver from colorectal cancer, neuroendocrine tumors, and even breast cancer.
Research on this and other new liver cancer treatments is ongoing. We are actively participating in The SIRFLOX Trial, which is evaluating radioembolization (Y-90) and chemotherapy in cancer involving the liver.
Dr. Facchini leads the VIR team in a liver radio-embolization procedure, one of the minimally invasive options for liver cancer treatments.
Often Y-90 therapy is used in combination with other modalities. One of the advantages of Y-90 treatment is the relatively low incidence of serious side effects and the fact that 95% of treatments are completely outpatient. The most common side effect is fatigue for several days. A full discussion of risks, benefits and alternatives for liver cancer treatments would take place at a patient’s consultation appointment.
Chemoembolization
For liver cancer treatments, hemoembolization offers an alternative to patients with primary or metastatic liver tumors that are unable to be surgically removed. This procedure involves placing a very small tube or catheter (photo) into the artery supplying the liver. The small vessels in the liver are then partially blocked with small particles (Drug eluting beads, or D.E.B.) carrying a mixture of chemotherapy. This technique delivers the chemotherapy into the tumor, so that it remains in the mass, greatly increasing the effective dose of chemotherapy while at the same time decreasing the toxicity to the rest of the body.
A tiny catheter used to deliver tumor-killing agents into the liver and other organs.
Thermal ablation
One of the newer techniques for liver cancer treatments, is being used by interventional oncologists for cancer treatment in Illinois and elsewhere to destroy cancer deposits deep in the body without invasive surgery. A thin needle is placed into a tumor using ultrasound guidance. Using either freezing technology, microwave energy, or radiofrequency energy, the tumor is destroyed. This technique is used for relatively small tumors in certain organs. We use these methods to treat tumors of the liver, kidney, spine and lung, most commonly.
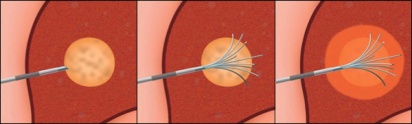
(Left) RFA probe entering a liver tumor. (Center) Energy-emitting tines emerge from the probe, inside the tumor. (Right) 3d Heat energy killing the tumor.

Cryotherapy for cancer Cryotherapy
Is used to freeze tumors, using imaging guidance. It is another effective local treatment of tumors that have not spread yet. Using image guidance, a tumor deep within the body is identified, localized in 3 dimesions with CT scanning or ultrasound, then small needles are placed painlessly through the skin (using local anesthesia and sedation) into the tumor. Liquid Argon gas is run through the needles, creating an iceball, freezing and killing the tumor, without invasive surgery.
Ice is seen forming on cryogenic tubes, carrying tumor killing power to small needles that are placed, with image guidance, to intersect into a kidney tumor. In this patient, the tumor was completely killed without stitches or sugery. The patient went home later that day.
A recent study of cryoablation of small kidney cancers showed “100% 5 year cancer-specific survival”,which approaches the “gold standard” of traditional surgical removal. In other words, invasive surgery is NOT better than cryotherapy for small kidney cancers
Additionally, patients with tumor deposits in the bone can undergo this therapy for pain relief.

Stenting
Stenting of Obstruction Caused by Cancer
In some patients, the tumors are large enough or invasive enough to block off the bile ducts, kidneys, colon, or esophagus. Patients with bile duct obstruction can be very uncomfortable due to pain, nausea and itching. Gastroenterologists may be able to pass a flexible metal stent to relieve the blockage. If they are unsuccessful, then, using X-ray guidance, an interventional radiologist can cross beyond the blockage and open a passage using balloon angioplasty and stent placement. Our doctors placed the first flexible metal stent into a human in our region, and have the longest experience with this procedure in the state of Illinois. Here, the main, right and left bile ducts have been opened up allowing the liver’s bile to flow freely into the intestine. Cancer had blocked the flow, but now the patient has “bionic bile ducts”, with the branching bile ducts armored with mesh-like tubular stents placed non-surgically. Bile duct stenting is palliative, but can allow longer life, outside the hospital. Kidneys can become blocked by tumors or kidney stones. The standard treatment involves an urologist bypassing the blockage from below through the bladder. If the blockage is too severe to be crossed in the standard fashion, an interventional radiologist can enter the kidney through the skin, placing a tube using ultrasound guidance. In the vast majority of patients, the blockage can then be crossed from above and a drainage tube (nephrostomy tube) or a ureteral stent placed to allow drainage of urine into the bladder. In the rare instance that the blockage is too severe, the interventional radiologist can place a tube in the kidney, which can drain the urine to the outside. Here, a patient with a colon cancer obstruction, who is too ill for open surgery, is treated using image guided placement of a colonic stent. The painful obstruction is relieved, without any surgery or risk of general anesthesia. Here, a colonic stent is seen (mesh-like structure within the colon) expanding the obstruction and relieving pain.

Biopsies
Image guided biopsy is the most common interventional cancer procedure. Our VIRChicago interventional radiologists will use CT or ultrasound scanning to guide a thin needle to painlessly sample a tumor or lymph node, avoiding unnecessary surgery.
Using CT scan guidance at VIR Chicago, a small diameter needle (placed using IV sedation) is used to obtain a painless biopsy of a nodule deep inside the body, without invasive surgery.
Cancer related pain relief procedures
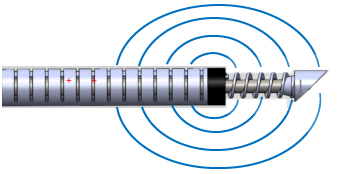
Interventional radiologists perform various procedures for pain control in cancer patients. Vertebroplasty and kyphoplasty can stabilize broken bones in the spine due to cancer deposits. ( More on spinal fractures). Radiofrequency ablation may allow a spine tumor to be destroyed with placement of a curved wand that emits energy.
A diagram of a steerable radiofrequency probe that can be placed through a needle, and guided with imaging, to deliver heat energy (oval blue lines) to cancer deposits in the spine. This can help to relieve cancer pain in the spine.
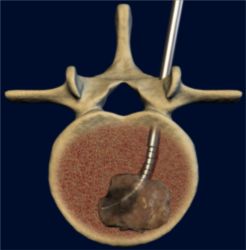
Here, a tumor in the spine is targeted for RFA heat destruction
Celiac plexus destruction can stop severe abdominal pain associated with some cancers. Radio-frequency ablation can be successful in stopping bone pain from tumor invasion outside the spine also.
Other Cancer related complications
In many patients with cancer, large amounts of fluid may accumulate in the chest cavity or in the abdomen. Using imaging guidance at our clinic in Illinois, our I.R. cancer treatment specialists can drain out the fluid with a needle or tiny tube (thoracentesis or paracentesis). If the fluid keeps returning, we may implant a Pleurex catheter to allow repeated, painless fluid drainage.
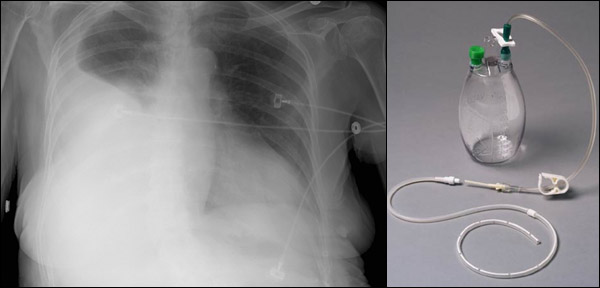
(Left) A chest x-ray shows a large fluid collection collapsing the right lung. (Right) A Pleurex catheter (lower tube with small side-holes) with separate disposable drainage system. The tube may be implanted in the IR department to relieve recurring fluid collections due to cancer.
We can work with your cancer physicians in consultation, to help bring the latest technology to bear in cases of cancer. We also have access toa network of elite specialists in other fields, such as Oncologic Surgery, Radiation Oncology, and Medical Oncology, to allow the best options for you, or your loved one.
For more information about possible candidacy for these cancer treatments, ask your family doctor or your oncologist.Contact us to learn more about a consultation for cancer treatment options offered by our physicians call (630) 856-7460.